As the call is made this World Health Day for global leaders to ensure health for all becomes a reality, the need to achieve universal health coverage (UHC) has never been so acute. Both in terms of addressing the growing burden of non-communicable diseases such as heart attacks and strokes which account for 71 per cent of all deaths globally, and in tackling and preventing the spread of infectious diseases such as influenza, Zika and Ebola.
As IDS Director Professor Melissa Leach highlighted on the anniversary of the Alma Ata Declaration which declared primary health care as critical to achieving health for all:
“To make progress towards the ambitious goal of Universal Health Coverage we must look beyond the technical aspects of health and foster even greater collaboration and coordination across sectors and disciplines, including the social sciences, to ensure that everyone can lead healthy lives, and has access to quality services and care”.
Strengthening health systems
As part of these collaborative efforts, there must be greater focus on strengthening health systems in order to achieve UHC. In a recent seminar given by Sinead Walsh (EU Ambassador to South Sudan) and Dr Oliver Johnson (Visiting Lecture at King’s College London) described how Sierra Leone’s ‘health system collapsed like a house of cards’ following the outbreak of Ebola. This was despite commitments made by donor and multilateral agencies to strengthen Sierra Leone’s health systems in the aftermath of the war which ended in 2002.
Indeed, following the outbreak, IDS researchers Dr Gerald Bloom and Hayley Macgregor underlined the critical importance of strengthening health systems, including the provision of widely accessible basic health services, to building people’s and societies’ resilience to future infections and their impact on livelihoods and economic development.
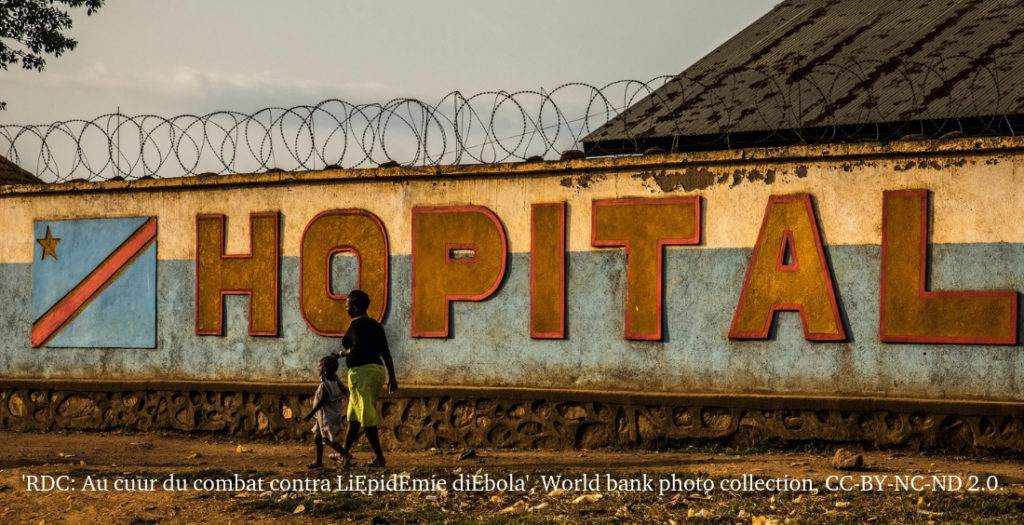
Global efforts have stepped up a gear in recent years. However, as recent events in Mozambique and the Democratic Republic of Congo (DRC) have demonstrated, countries with weak health systems as well as high levels of poverty and histories of violence and conflict continue to struggle to cope in the face of the intense demands of a disease outbreak or pandemic. In DRC the current Ebola outbreak has killed 679 people and following Cyclone Idai, there has been a growth in cases of cholera and the first death reported from the disease in Mozambique.
Looking beyond technical solutions to health challenges
Too often global health responses to issues such as disease ‘preparedness’ or antimicrobial resistance (AMR) which remain key obstacles to achieving UHC, have been overly focused on technical solutions. For example, researchers, who are part of the Pandemic Preparedness programme funded by the Wellcome Trust have argued disease preparedness strategies are concerned with drugs, vaccines, surveillance systems and scenario planning exercises but do not sufficiently take account of how communities anticipate and manage disease, as well as take account of a broader set of risks including precarious livelihoods, natural disasters and conflict.
Moreover, initiatives to tackle antimicrobial resistance (AMR) have largely centred on creating new antibiotics and undertaking antibiotic resistance surveillance. Yet many of the problems around AMR arise from the misuse and misdiagnosis of antibiotics which may increase the risk of drug resistance. As Dr Gerald Bloom and Tom Barker argue effort and resources also need to be invested in ensuring better regulation of the informal markets through which antibiotics to treat infections in both humans and animals are distributed, as well as promoting understanding of the effective use of antibiotics amongst the public and health workers.
An example of a more holistic approach that brings together different sectors and disciplines to tackle these issues is new work been done through the UK Research and Innovation (UKRI) Global Research One Health Poultry Hub. The hub, led by the Royal Veterinary College and including a number of IDS researchers, will address the need to meet rising demands for poultry meat and eggs in developing countries, while minimising risk to international public health through threats including bacterial food poisoning, strains of avian influenza with epidemic or pandemic potential and increased antimicrobial resistance.
Accountability for Health Equity
This cross-sectoral and multi-disciplinary approach to understanding the barriers to achieving universal health coverage is also integral to one of the other UKRI Global Research Hubs that IDS is involved with. The Accountability for Informal Urban Equity Hub (ARISE) led by Liverpool School of Tropical Medicine will support marginalised people to claim their rights to health in Sierra Leone, Bangladesh, Kenya and India and build government accountability and capacity to provide citizens with security and services.
Strengthening accountability was also explored in more detail in the IDS Bulletin issue (funded by the Impact Initiative) Accountability for Health Equity: Galvanising a Movement for Universal Coverage. In this issue, academic, activist and civil society authors argued that greater priority needs to be given to building links and facilitating dialogue across sectors and levels of decision-making and with communities such as indigenous peoples to understand how greater accountability can be achieved.